AI agents at work
– 7 min read
Your coverage letters are fueling friction — and it’s hitting your member experience metrics

A single coverage decision letter can set off a chain reaction. In the US, health insurers adjudicate more than 3 billion medical claims each year, sending millions of letters every month, each one carrying legal and human weight. Yet too often, they confuse more than they clarify — and that confusion shows up everywhere in your operation.
When members don’t understand a decision, they don’t act. They delay care, call for help, or abandon the process altogether. Each point of confusion becomes another touchpoint for your service team. Another call, another escalation, another preventable cost. With one survey estimating the average annual cost of operating a healthcare call center to be $13.9 million, even small increases in call volume add millions in overhead.
The role of AI in fixing friction
I’ve learned that fixing friction isn’t just about better writing — it’s about better systems. That’s why I see AI not as an add-on, but as the only scalable way to solve this problem at its root.
Every payor I work with faces the same pattern: thousands of letter templates, all manually edited, reviewed, and distributed. Even with great people and good intentions, clarity always collapses at scale. Letter writers spend hours searching through policy documents, benefit codes, and regulatory language — just to find the right wording for one case. The result is variation, delays, and frustration on both sides.
AI is uniquely suited to manage that complexity: it can surface the right policy context, apply approved phrasing, and keep everything aligned with compliance. With the right guardrails, AI enforces plain-language principles, carries approved phrasing across every channel, and keeps compliance language intact — automatically. It frees teams from manual rewrites and lets them focus where human judgment truly matters: resolving exceptions, improving experience, and rebuilding trust.

Exploring the ways AI can work for your team?
Read more about how AI agents work in healthcare
The system-level impact
The real opportunity here isn’t found within any one letter. It’s about creating a system that consistently delivers clarity, no matter who writes, reviews, or sends it. When you build that kind of repeatable model — powered by AI and grounded in compliance — the results show up everywhere that matters:
- Appeals drop because members understand what to do.
- Call volumes decline because fewer people need help interpreting next steps.
- Compliance risk decreases because approved language stays consistent across templates and states.
- Member satisfaction rises not because the message changed, but because the experience did.
That’s what I mean when I talk about friction you can’t afford. It’s not just financial waste, it’s operational drag that erodes trust and drains teams. Eliminating it isn’t about writing better letters; it’s about building a smarter system for all your communications.
When clarity fails, care fails
I’ve seen firsthand how these breakdowns play out. A member receives a denial letter full of technical language. They reread it three times, still unsure whether it’s final, whether they can appeal, or how long they have. Days pass. The appeal window closes. Care gets delayed, sometimes for weeks, sometimes indefinitely.
That moment isn’t just frustrating – it’s dehumanizing. It tells people that the system designed to help them isn’t built for them at all. And for payors, that loss of trust doesn’t just hurt the member relationship; it undermines the entire mission of access and care.
When clarity fails, it fails on multiple levels. The member feels unheard. The clinician gets stuck in back-and-forths. The call center absorbs the overflow. And leadership ends up managing the consequences instead of preventing them.
Clear, consistent communication isn’t about optics. It’s a core operational function that protects the integrity of every member interaction.
The data behind the friction
If you want proof that friction starts with communication, just look at the numbers. More than half of all US adults read below a sixth-grade level, with ~45million considered functionally illiterate, reading below a fifth-grade level. When members can’t parse the sentences in medical letters, it’s not just a matter of confusion — it’s exclusion.
When appeals are necessary, the wait only deepens the impact. A typical appeal can take 30 to 60 days to resolve, leaving members in limbo, uncertain whether treatment will move forward or be delayed indefinitely. That waiting period is more than administrative time; it’s prolonged stress and risk for the member, and reputational risk for the plan.
Across the industry, only about one in ten denials are appealed, even though more than 80 percent of appeals succeed. That gap represents a simple truth: unclear communication stops people from acting — it withholds care. But the solution isn’t empathy training or call-center expansion, it’s clarity, delivered consistently and at scale.
Where clarity breaks down — and how to rebuild it
In every plan I’ve worked with, the same pattern repeats — letters satisfy compliance, not serve people. Decisions get buried in dense text. Next steps get reduced to vague guidance like “You may appeal.” Appeal rights vary by state, and language drifts across templates and channels. None of this is malicious — it’s structural. Legacy systems and regulatory pressures have turned clarity into a compliance checkbox instead of a design principle.
The most effective payor communications don’t succeed because they’re well-written — they succeed because they use predictable patterns of clarity. Every sentence earns its place. Every decision and next step is unmistakable. Consistency becomes a form of care.
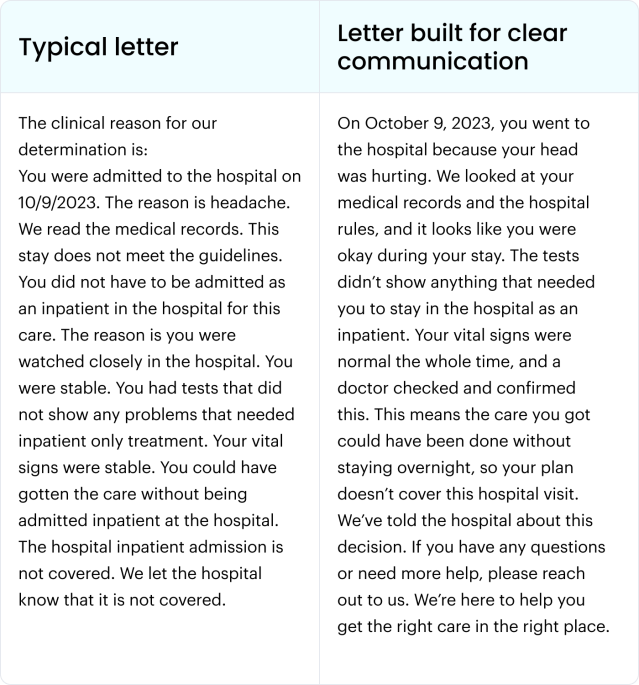
That’s what needs to change at scale: moving from documentation to direction. The goal isn’t to make letters sound kinder — it’s to make them clear, clinically grounded, and human enough for every member to understand and act on. AI makes that shift possible — not by automating empathy, but by making clarity operational and repeatable.
Scaling clarity in action
A single clear message can change an entire experience. When a member reads a denial and immediately understands the decision and what to do next, that’s clarity working as it should.
At scale, that clarity can be maintained by a regulatory-grade AI framework. Unlike commercial generative AI that can devolve into endless prompting and manual rewriting, this kind of framework combines generative and agentic AI with governance, auditability, and jurisdictional rule enforcement. The result is a system that doesn’t just generate text; it creates defensible, reusable, and compliant communications at enterprise scale.
Once a claim determination is made, the AI framework draws information directly from connected systems — policy language, clinical rationale, and member data — and checks it against brand, compliance, and jurisdictional guardrails. It then produces a complete, compassionate, and compliant letter, ready for human-in-the-loop approval and printing.
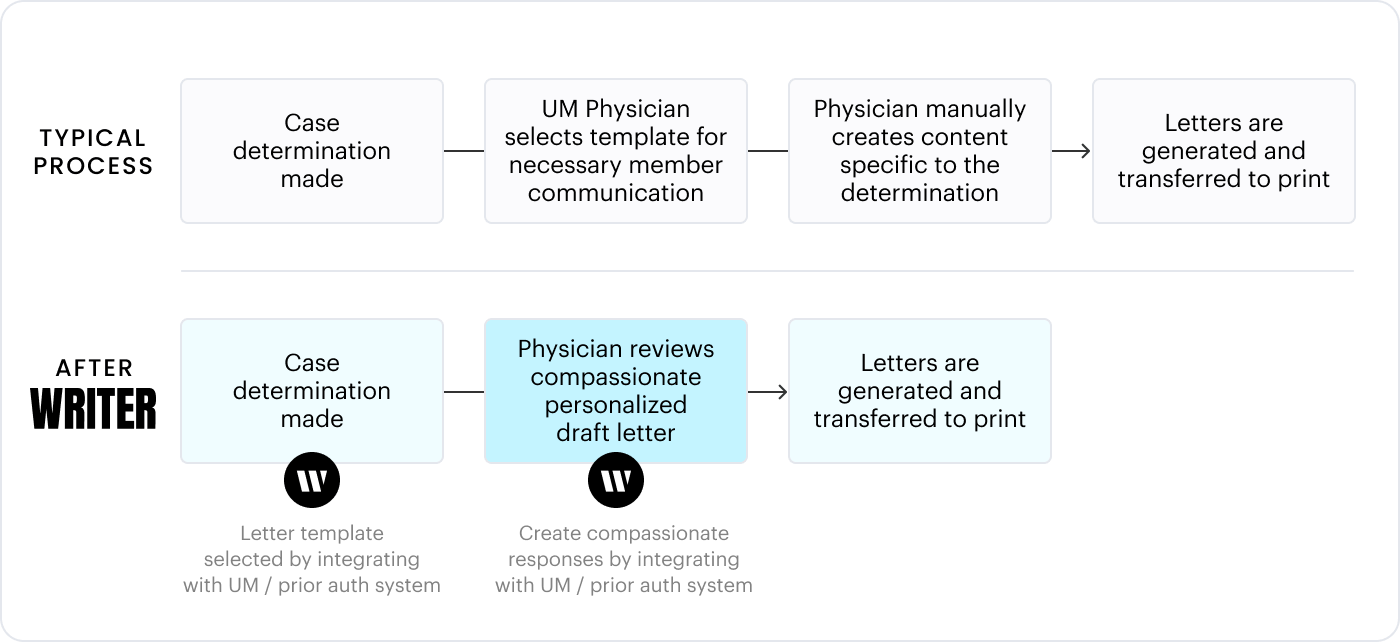
Because the framework sits at the system level, every update — whether a new benefit rule, clinical guideline, or jurisdictional requirement — automatically propagates across all communications, keeping the entire organization aligned and compliant.
That’s what scaling clarity looks like in practice. It’s not only faster because it’s automated; it’s faster because it’s aligned — powered by a framework that blends machine precision with human oversight to ensure every communication is accurate, compliant, and worthy of member trust.
From friction to confidence
Every time a letter prevents a call, closes an appeal loop, or keeps a member in care, it proves your system works the way it should. The results are easy to see, and they ripple across every part of the organization:
- Fewer appeals mean reduced legal and service costs.
- Fewer calls mean leaner operations and less strain on your teams.
- Consistent messaging reduces compliance exposure.
But the real gain isn’t efficiency — it’s confidence. When members understand their decisions, they act faster, stay in care, and trust the process. When teams don’t have to rewrite, chase, or explain, they focus on what matters most: helping people get the care they’re entitled to.
That’s what clarity at scale delivers. Not letters that document, but communications that direct. Not a system that reacts, but one that leads — with transparency, consistency, and trust, powered by people and sustained by AI.
If you’d like to find out more about how clarity and trust-first communication scale across healthcare, explore our healthcare solutions page.