Inside WRITER
– 4 min read
From months to moments: IBM and WRITER’s AI solution modernizes healthcare communications
A single member letter can set off a costly chain reaction. In the US, health insurers send millions of these communications every month, each one carrying significant legal and human weight. Yet too often, they confuse more than they clarify, creating friction that ripples across the entire operation. When members don’t understand a coverage decision, they delay care, overwhelm call centers, and lose trust in the system designed to help them.
This isn’t a simple writing problem; it’s a systemic one. For decades, health plans have been hampered by organizational silos, fragmented data, and legacy technology, making the path to clear, consistent communication feel like an insurmountable climb.
But what if you could move from months to moments? A new strategic partnership between IBM and WRITER is set to transform this critical function, offering a simplified, scalable path to enterprise AI that solves healthcare’s most pressing operational and experiential challenges.
An AI-powered partnership to break down silos and build trust
The challenge for healthcare organizations is clear. According to Melissa Geissler, Partner for Public Market Customer Strategy & Operations at IBM, the core issues are about breaking down deep-seated organizational silos and finding ways to engender trust in every single member interaction. While many health plans have the appetite to move fast into the future with generative AI, they are often unsure where to start or how to achieve real business outcomes at scale.
This uncertainty leads many to invest in niche solutions that only address pieces of a process, rather than rethinking the fundamental interaction between people, process, and platforms.
This is where the IBM and WRITER partnership creates a unique advantage. It combines IBM’s deep industry expertise—spanning decades of work in healthcare data, legacy systems, and generative AI strategy—with WRITER’s full-stack, secure AI platform. The synergy provides a powerful, value-oriented approach that doesn’t require ripping and replacing existing systems. Instead, it amplifies the value of platforms organizations have already invested in, supercharging workflows and connecting disparate systems.
“What makes me really excited is that the future-state capabilities and the vision we’ve been talking about for years, WRITER helps make real on very accelerated timelines. WRITER is able to come in, connect workflows, and be that agentic backbone that makes the aspirations of an organization much more real.”
In focus: The AI solution to transform member communications
Nowhere is the potential for impact clearer than in member and provider communications. This area has long been a source of “structural friction,” plagued by manual workflows and a dizzying volume of templates. Geissler notes that for many organizations, the complexity has felt like “too steep of a hill to climb to get started,” with some health plans needing weeks of development just to launch new templates to meet state regulations.
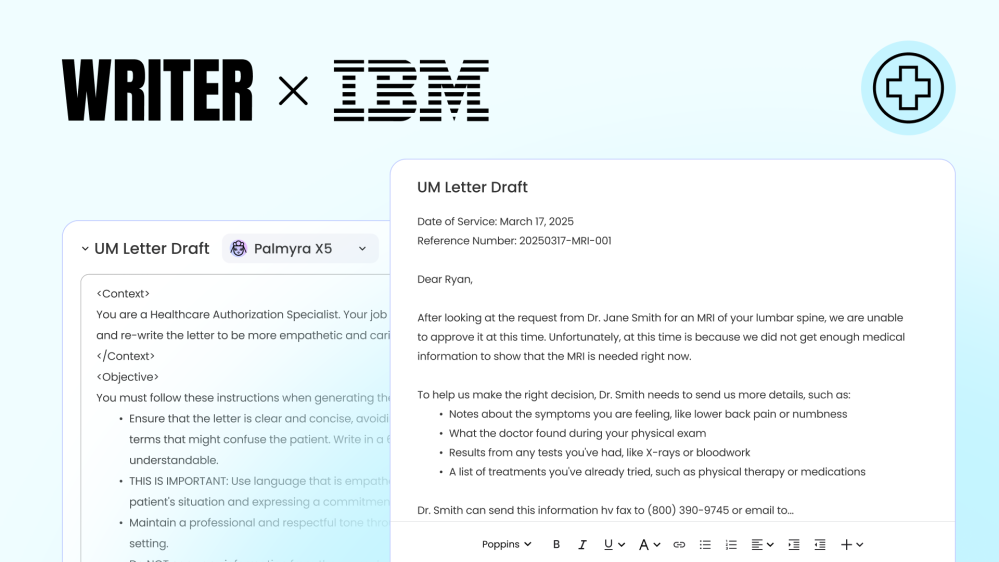
The IBM and WRITER solution for personalized communications directly addresses this pain point. It moves beyond the status quo by empowering business users to create, manage, and personalize compliant communications in days, not months. The key is a system-level approach. Instead of manual rewrites, the platform uses a regulatory-grade AI framework with built-in governance and auditability. It codifies compliance rules, connects to policy language and member data, and checks every communication against brand and jurisdictional guardrails. The result is a complete, compassionate, and compliant letter, ready for human-in-the-loop approval.
This allows organizations to finally move past the inertia of their complex legacy systems and accelerate their traditional workflows in a secure and compliant manner.
The human impact: When an AI solution drives clearer care
While the operational wins—like reduced call volumes and fewer appeals—are significant, the human impact is even more profound. Every healthcare user can relate to receiving a confusing communication that leaves them wondering what to do next. This problem is only exacerbated for members with more complex health issues, where any friction can undermine their health and wellbeing.
By transforming confusing documentation into clear, actionable guidance, the partnership helps rebuild the fragile trust between members and their health plans. When a member understands a decision and their next steps, they’re more likely to get the right care in the right place. This creates a virtuous cycle: a better-supported member is part of a stickier, long-lasting relationship, which is the ultimate goal for health plans.
A scalable AI future, today
The journey to better member and employee experiences is ongoing, but the path forward is clearer than ever. The IBM and WRITER partnership is about more than just technology; it’s about creating a scalable model for transformation that connects people, processes, and platforms to drive meaningful change—and to do it fast.
“I really think that we are pulling the right people, relationships, and technologies together to make anything possible. It’s not about creating highly customized solutions. It’s about creating things that can really scale.”
Ready to move from months to moments in your member communications? Learn more about our healthcare solutions or request a demo to see the IBM and WRITER solution in action.




