The big book of
AI agents for
healthcare payors
Introduction
Healthcare is an industry fraught with complexities and cumbersome administrative tasks that can often overshadow the critical goal of patient care. For today’s healthcare payors and risk-bearing providers, there’s only one solution: Invest in AI systems that drive meaningful clinical impact at scale. While there’s no one-size-fits-all solution for all conditions and populations, agentic AI is the key to building highly impactful, clinically relevant, and cost-effective solutions.
Agentic AI is a type of advanced AI that combines skills like research, analysis, translation, and code generation to perform complex, multi-step tasks. AI agents deliver accurate and consistent outputs grounded in your data — making them invaluable for improving work, reducing errors, and enhancing overall efficiency.
While the rapid advancement of AI can be daunting — especially for organizations that have yet to see meaningful results from generative AI — the potential of agentic AI is already here and should be embraced. Building, activating, and supervising AI agents at scale requires a collaborative effort between IT and business teams. This isn’t just about automating simple tasks anymore. It’s about building agents you can direct to help your business achieve outcomes quickly and accurately.
This is especially true for national-scale players who need to manage vast and diverse populations efficiently and effectively. By embracing these early stages of agentic AI, healthcare organizations can lay a solid foundation for future advancements. This ensures they stay ahead of the curve in an increasingly competitive and technology-driven landscape.
Download the ebook
Current challenges in healthcare
The healthcare industry is grappling with complex issues that hinder operational efficiency and patient outcomes. Some of the most pressing challenges are:
- Regulatory and payment complexity: A web of regulatory frameworks and payment systems adds layers of bureaucracy, making the simplest tasks complicated and hard to navigate.
- Economic incentives and siloed systems: Conflicting incentives lead to institutional silos and a proliferation of technologies that don’t work well together and slow teams down.
- Rapidly expanding medical knowledge: Medical knowledge is growing so fast that it’s nearly impossible for healthcare professionals to keep up with the latest standards and discoveries.
- Administrative burden on healthcare workers: Highly educated and dedicated healthcare workers spend countless hours on administrative work, leading to frustration and burnout.
These challenges have culminated in unsustainable healthcare costs, dissatisfied patients, and poor patient outcomes. A demoralized workforce adds to the strain, making finding solutions that can improve processes and care imperative.
Why agentic AI is the solution
Agentic AI can uniquely address some of the most important underlying problems in healthcare: information overload and overwhelming complexity.
Through well-designed and well-executed AI systems, healthcare personnel can operate at their full potential to maximize human health, financial performance, and personal fulfillment at work. In so doing, they can capitalize on this once-in-a-generation opportunity to broadly transform their work for patients and healthcare systems.
Transforming health plan workflows with agentic AI
Member & provider support
Efficient, tailored support to ensure seamless assistance for members and providers
Claims & payment processing
Streamlined claims processing for faster reimbursement & greater payment transparency
Population health & risk management
Improve health outcomes & manage risks through data-driven population health strategies and actuarial insights
Provider relations & contracting
Optimize provider networks, contracts, and partnerships to ensure quality, cost-effective care
Care mgmt. & utilization mgmt.
Personalized care and utilization management to ensure members get the right care at the right time
Benefit plan design
Customized health coverage to meet member needs, control costs, and drive differentiation
Core enabling services
Ensures seamless operations across key support services to drive efficiency, compliance & growth
This guide will show you the transformative power of agentic AI for healthcare payors. From reducing administrative costs and boosting member engagement to analyzing complex member data, “The big book of agentic AI use cases for healthcare payors” provides practical use cases and a path to get started. This resource will empower you to use AI to enhance efficiency, elevate the quality of care, and maximize outcomes — ultimately driving greater value for your organization and the members you serve.
The five-level path to agentic AI transformation in healthcare
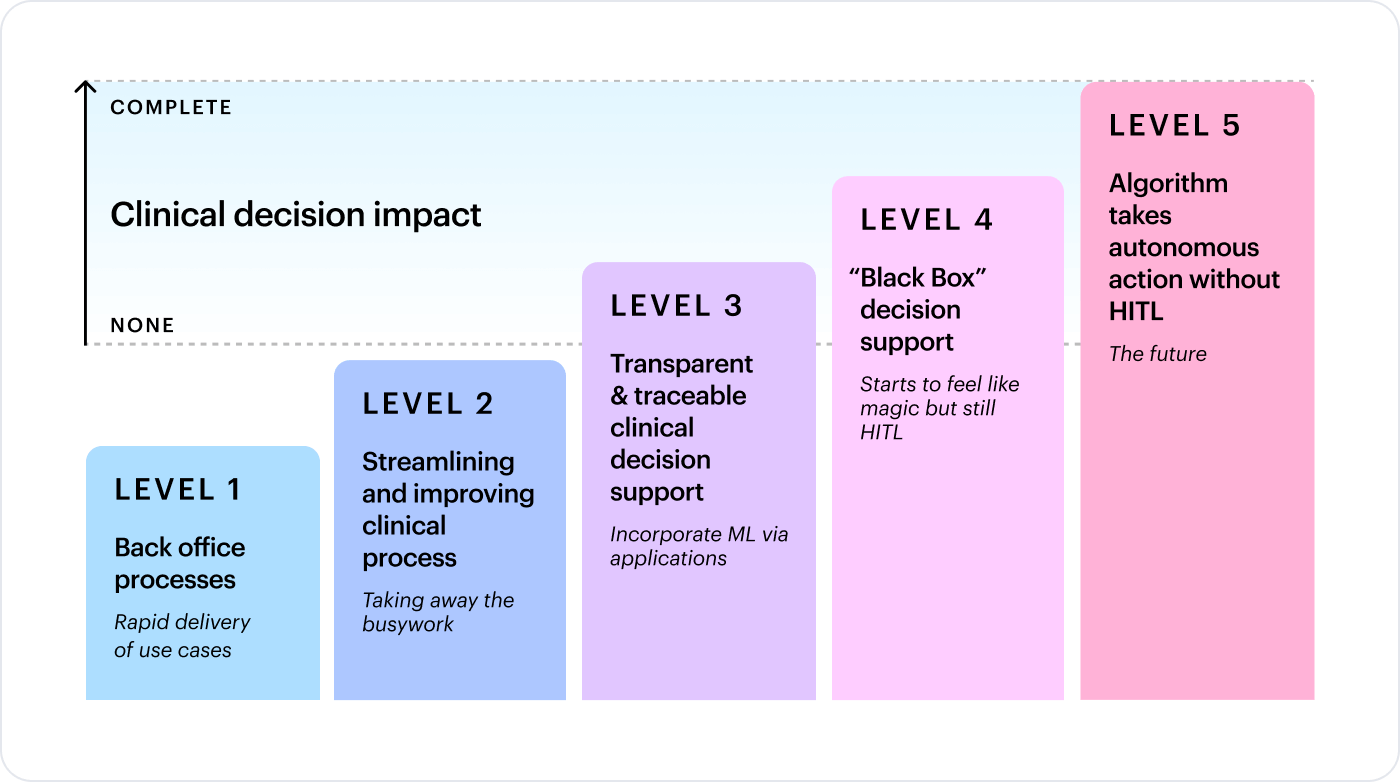
Agentic AI transformation in healthcare won’t happen overnight. LLM outputs are non-deterministic. The risk of hallucinations is too great when patient data and patient care are at stake.
In these early stages of agentic AI, think of the path to AI transformation in five levels. Use cases at early levels pose no risk to patients, and each advancing level requires more and more human oversight. Today, most healthcare organizations, including healthcare payors, are only ready for agentic AI at levels one and two, from back-office processes to improving clinical processes. More sophisticated organizations may be experimenting with agentic AI in clinical decision support.
Agentic AI use cases for healthcare payors
In the rest of this guide, we explore five example use cases across levels one through three, where we see payors using agentic AI today.
Level
Example use cases
Level 1
Back-office processes
- Customized RFP generation
- Compliant marketing content creation
Level 2
Clinical process
- Provider network adequacy and contract drafting
Level 3
Clinical decision support
- Prior auth decision support
- Clinical documentation and coding review
Level 1
Level 1
Level one use cases focus on back-office processes with no clinicians or clinical decision-making involved. There’s no risk to patients or patient data. The level of validation is lowest here while enabling rapid delivery of agentic AI use cases and ROI to help organizations and AI leaders more quickly prove the business value.
Agentic AI use case: Customized RFP generation
Every year, health insurers and third-party administrators (TPAs) respond to thousands of RFPs — each requiring extensive customization based on industry, geography, and demographics. This manual process can involve dozens of people working for weeks. The complexity and resource intensity of updating RFPs, making bid/no-bid decisions, and coordinating across multiple teams can be overwhelming.
Agentic AI improves this process by automating and doing the heavy lifting across key steps. For example, an agentic workflow can automatically connect to your CRM system, like Salesforce. When you receive an RFP, details get instantly fed into your CRM. This saves teams time and creates efficiencies — especially when handling hundreds or thousands of RFPs annually. Agentic AI supports bid/no-bid decisions by analyzing past success rates and customer insights, optimizing your RFP strategy. Finally, an agentic AI workflow will draft the RFP response for human review, making the RFP process more efficient, more cost-effective, and even less error-prone.
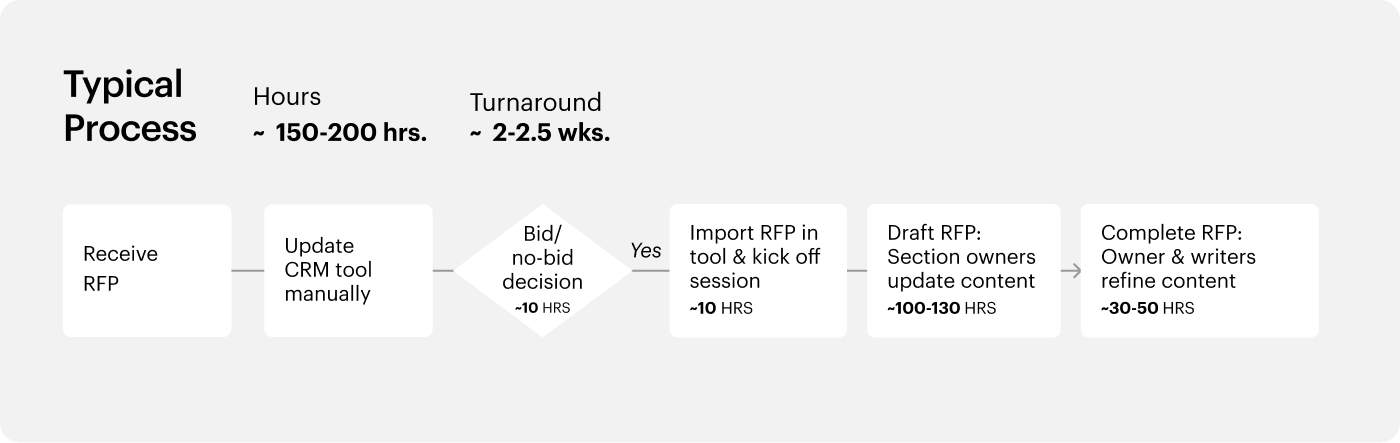
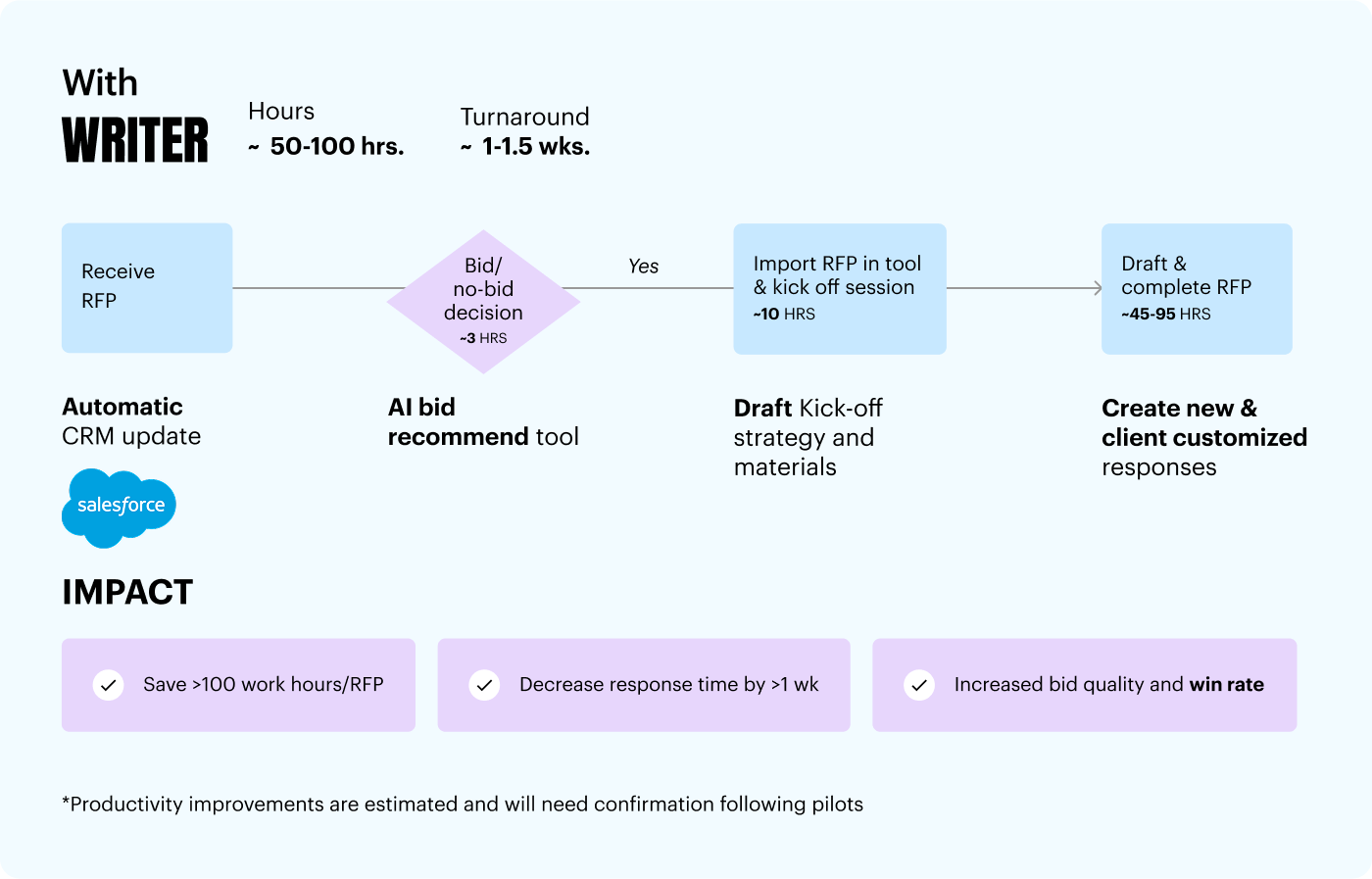
Example: A health plan receives an RFP from a large hospital network requesting detailed information on health insurance plans, coverage options, and specialized services. An agentic AI workflow extracts relevant information and updates Salesforce, then analyzes the RFP to help the team quickly decide whether to bid. If the decision is to bid, an AI agent generates an initial response using a knowledge base of past proposals and source documents. The draft is automatically sent to the team via Microsoft Teams for review and customization. This agentic AI workflow reduces completion time from weeks to days, resulting in faster decision-making, higher response quality, and an increased win rate.
Agentic AI use case: Compliant marketing content creation
In the competitive market for Medicare Advantage and employer-based insurance, health plans face the challenge of creating marketing content within a short window. Complex approval processes often slow this down. By integrating agentic AI into the content development process, health plans can generate highly personalized and compliant content 10 times more effectively and in just a quarter of the usual cycle time.
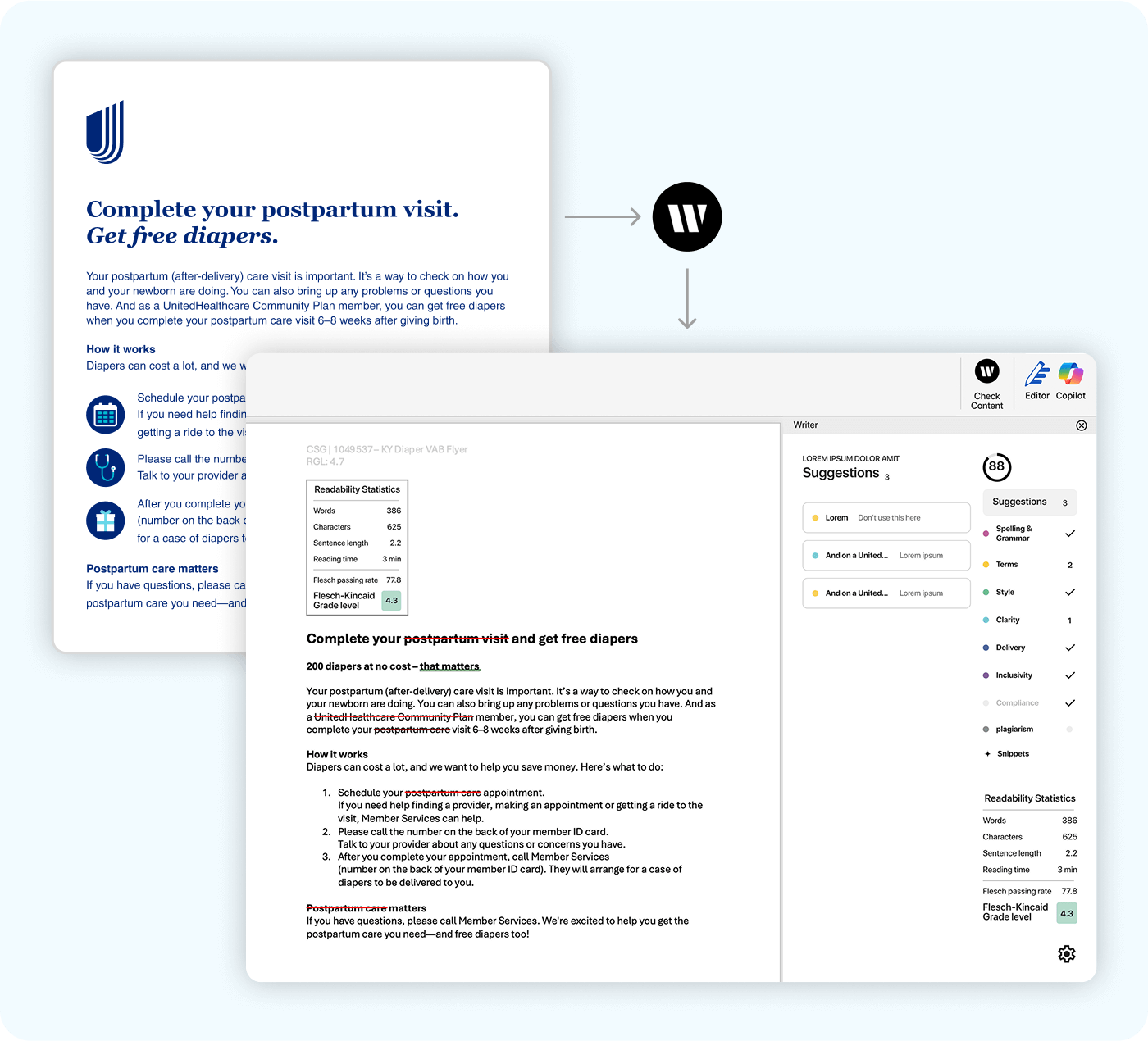
Example: A healthcare organization faces the challenge of making sure that their Medicaid marketing materials meet readability guidelines (RGL) mandated by many US states. The process of obtaining Flesch-Kincaid scores to confirm readability is manual, labor-intensive, and can cost anywhere between tens and hundreds of dollars per document from an external agency. This delays marketing timelines, and risks state fines for noncompliance.
To address this, the organization uses an AI agent to automate the RGL process. An AI agent generates compliant documents with crossed-out, ignored terms and grade-level confirmation, ready for state submission. This agentic workflow significantly reduces costs, accelerates marketing timelines, and minimizes the risk of noncompliance.
Level 2
Level 2
Level two use cases help smooth and improve clinical processes, freeing up clinicians from administrative work to focus more on patient care. There’s still no clinical decision support here, and again poses minimal risk to patient data or patient care.
Agentic AI use case: Provider network adequacy and contract drafting
Healthcare payors often struggle with communicating provider network adequacy — a very manual process involving extensive analysis of spreadsheets, provider outreach, and navigating complex regulatory requirements. This can lead to significant delays and errors that make meeting state-mandated provider access standards challenging. Agentic AI can address these pain points by analyzing provider rosters, claim volumes, and appointment availability to identify care access gaps. It can generate targeted outreach language, draft initial provider contracts, and ensure regulatory compliance. Plus, AI can automate adequacy reports, improving regulatory submissions.
Example: A Medicaid plan operating in rural counties struggles to meet state-mandated provider access requirements. An agentic AI workflow can quickly scan provider rosters and claim volumes, identifying zip codes and specialties with gaps in care access. It then generates targeted outreach emails and talking points for the recruitment team to use when contacting these potential providers. Once a provider is engaged, an AI agent drafts initial contract templates and checks them against state and federal regulations to ensure compliance. Finally, AI can automate the creation of adequacy reports, making the submission process to CMS and state agencies faster and more accurate. This approach saves time, reduces errors, and ensures members have better healthcare access.
Level 3
Level 3
Level three use cases are the first set of use cases where AI is used to support clinicians in making decisions that impact patients. But outputs from AI must be fully traceable because the clinician must stay in the loop, and ultimately bear responsibility for the outcome and the impact on patients.
Agentic AI use case: Prior auth decision support
Delays in prior authorization for high-cost procedures like surgeries and MRIs can be a significant source of frustration and anxiety for patients. This leads to prolonged wait times and potential harm if treatment gets postponed. For healthcare providers, the process is time-consuming and resource-intensive, causing administrative bottlenecks and increased costs.
AI agents can help by automating the extraction and summarization of patient data from EHRs, retrieving relevant rules and guidelines, and conducting a preliminary criteria assessment. Agents can also improve the communication process by generating more compassionate and patient-friendly letters that clearly explain and use supportive language. This reduces administrative burdens, cuts costs, and ensures better care, improving the overall healthcare journey.
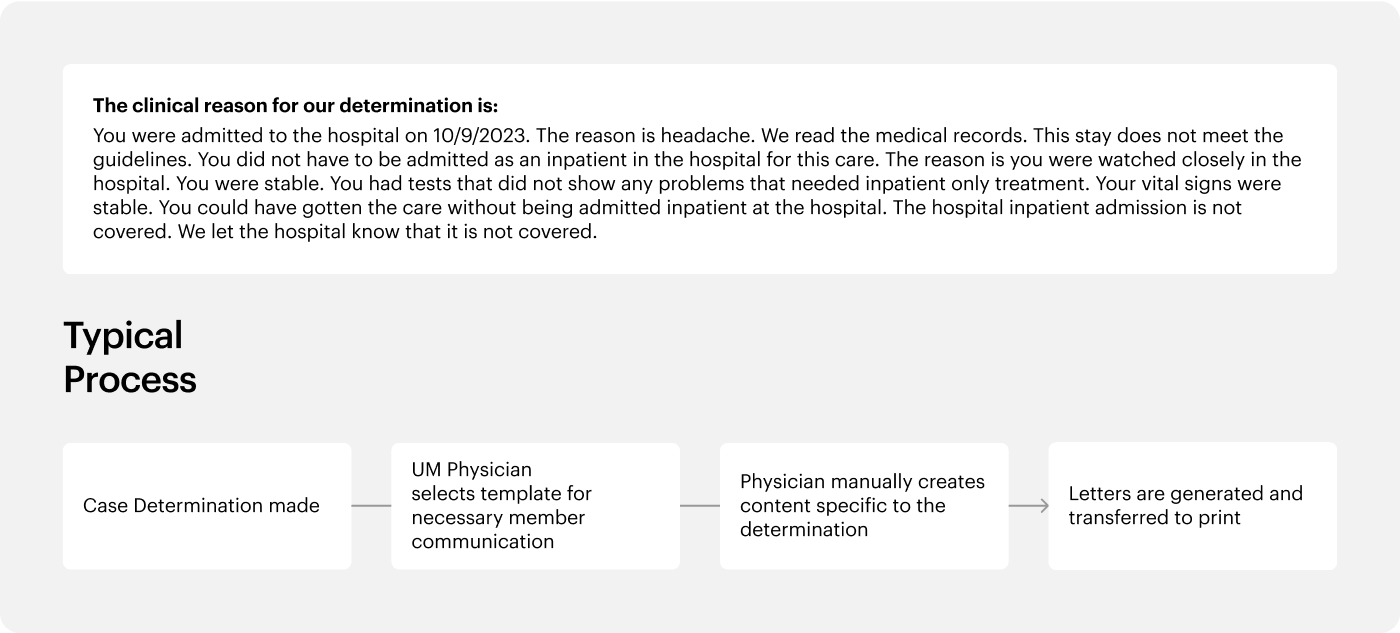
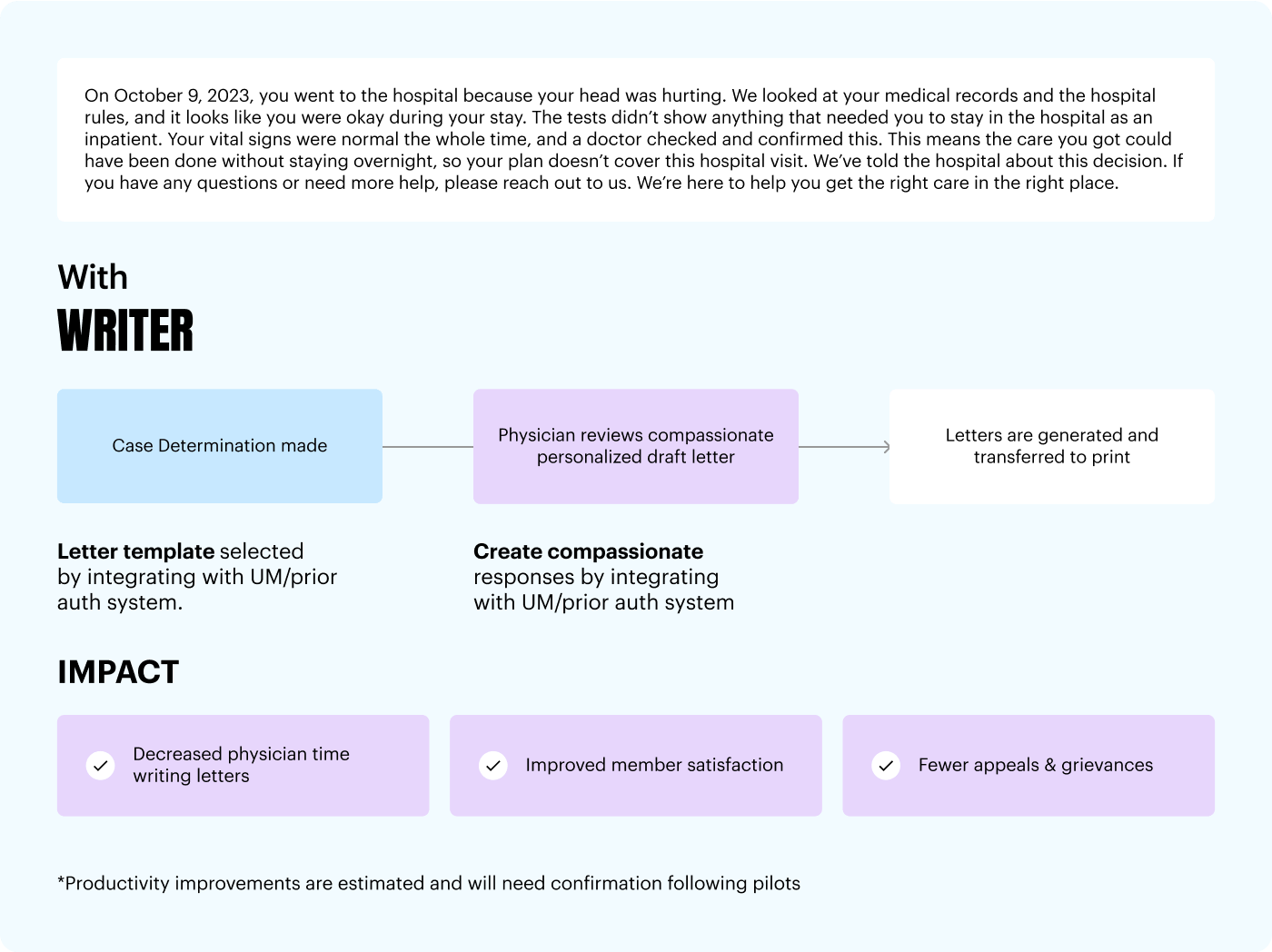
Example: A healthcare payor receives a request for prior authorization for an MRI for a patient with severe chest pain. An AI agent can pull and summarize the patient’s medical history from the EHR, compare it with insurance guidelines, and conduct a preliminary assessment. An AI agent can then generate a compassionate and clear letter to the patient, whether the MRI is approved or denied, which is reviewed by a medical reviewer for final approval. This streamlined process reduces wait times, ensures consistent and transparent decisions, and allows the healthcare team to focus more on patient care.
Use case: Clinical documentation and coding review
Accurate clinical documentation is essential for risk adjustment, reimbursement, and compliance — not just in Medicare Advantage but also in Medicaid, ACA Exchange, and Commercial plans. Yet today, many healthcare payors still rely on manual chart reviews that are time-consuming, error-prone, and costly. Missed or unsupported diagnoses can lead to revenue loss, audit exposure, and inaccurate patient profiles. Agentic AI changes that by reviewing provider notes at scale, surfacing coding gaps, and aligning documentation with regulatory and plan-specific criteria. The result: more accurate risk scores, reduced audit costs, and a clearer picture of each member’s health status.
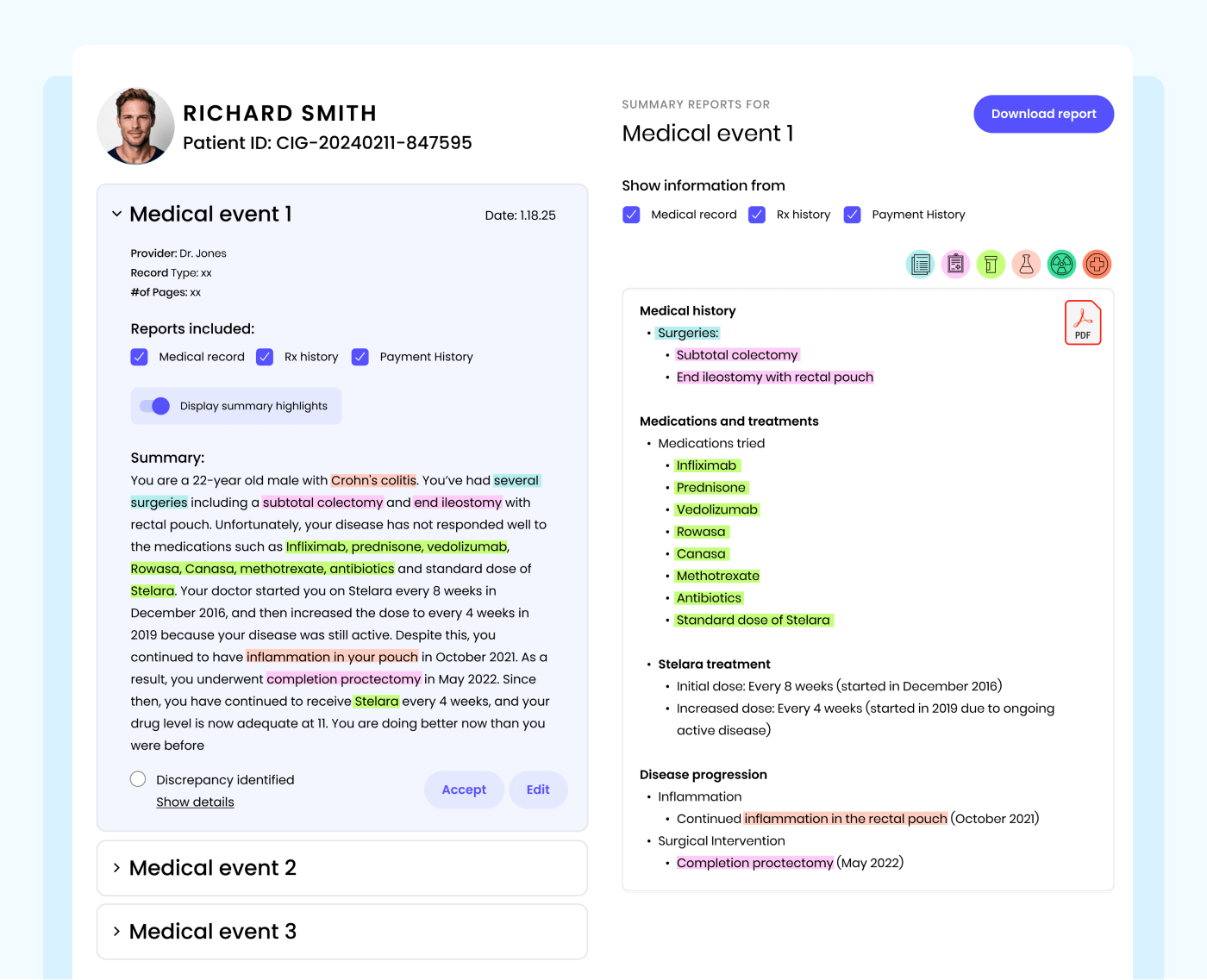
Example: A national health plan uses Agentic AI to review a 200-page medical record. The AI identifies that the patient has been prescribed Metformin, but the note doesn’t clearly document the diabetes diagnosis. It flags this discrepancy and suggests appropriate coding adjustments. The plan addresses the gap proactively — reducing audit risk, improving risk capture, and helping ensure that the member’s clinical record reflects their true health needs. This leads to more personalized and effective care.
Considerations in adopting agentic AI for healthcare payors
Even though we’re in the early days of agentic AI, the technology is already capable of transforming operations — from back-office processes to clinical decision support. However, successfully implementing agentic AI in healthcare organizations requires navigating complex people, process, and technology considerations to ensure meaningful impact. Despite the significant potential benefits, decision-makers should carefully evaluate these challenges to mitigate risk and ensure high-quality and impactful engagement with HCPs, patients, and regulators.
Accuracy and reliability
High-profile inaccuracies and AI “hallucinations” from consumer-grade systems have understandably shaken the confidence of healthcare leaders. Many are unaware of the advanced accuracy and reliability offered by enterprise-grade and medical-specific agentic AI solutions. Retrieval augmented generation (RAG) solutions that are grounded in your data integrate context-specific information while maintaining data integrity. AI should also offer transparency and traceability in outputs, ensuring that all generated content is cited and can be easily verified.
Trust, privacy, and security
Given the sensitivities around patient data and stringent regulations governing healthcare, security is paramount. However, many agentic AI solutions lack the security capabilities to meet strict requirements. As you evaluate partners, ensure that your company’s data is never shared or used for model training and that there’s a zero-day retention policy on your data.
Cross-enterprise platform
The surge of existing solutions adding AI capabilities, coupled with new AI-native solutions that don’t integrate leads to governance issues and exacerbates silos. This results in fragmented processes and adoption challenges. Deploying agentic AI today requires organization-wide coordination between business users — who are closest to the requirements — and IT teams, who need to manage security, integrations, and the total cost of ownership.
AI program management
Healthcare workers may resist AI due to fear of the unknown. They can lack the time or incentives to independently learn about and integrate agentic AI into their workflows. Leaders at the highest levels of the organization should champion AI evangelism, formalize and continue education, and incentivize and track usage. Consumer-grade UX and tool design help accelerate adoption. Find partners who are experts in agentic AI change management and delivery to accelerate impact and adoption.
How to evaluate LLM and generative AI vendors for enterprise solutions
learn more on the blog
WRITER is the end-to-end platform for scaling agentic AI in the enterprise
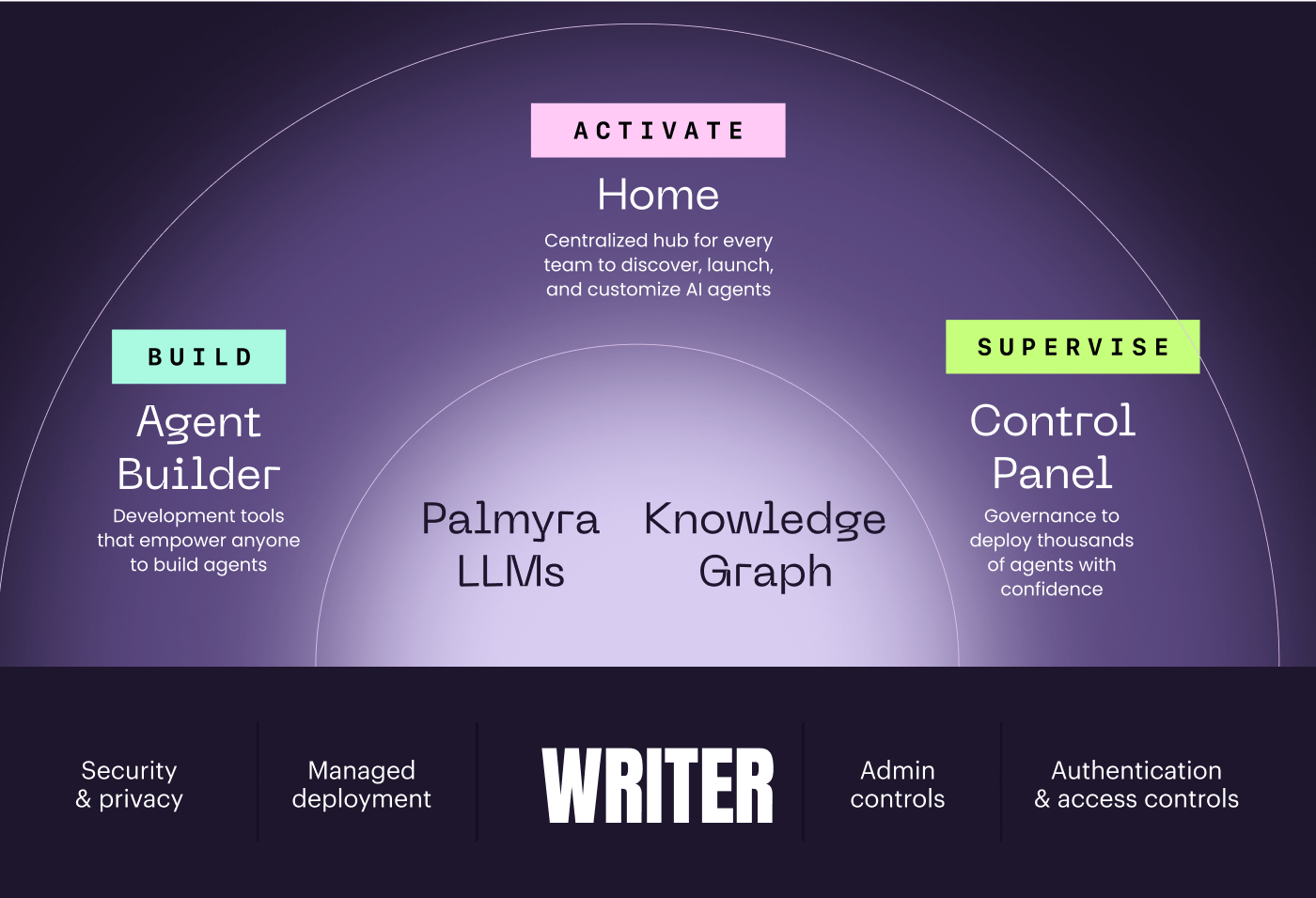
At WRITER, we understand the unique challenges and requirements of the healthcare industry. We empower enterprises to create their AI HQ — where IT and business collaborate to build, activate, and supervise AI agents together without compromise, all in one place.
WRITER is powered by:
- Palmyra LLMs, purpose-built for enterprises and the healthcare industry
- Knowledge Graph, our graph-based RAG solution that reliably and securely integrates your data
- Agent Builder to rebuild processes from the ground up — all under IT governance
- A consumer-grade experience that accelerates adoption
- Comprehensive program management to guide you on your agentic AI journey